Research Article - Der Pharma Chemica ( 2017) Volume 9, Issue 3
Sealing of the Implants in Orthopedy: Which are the Selection Criteria?
Adnane Benmoussa1, Hakim El Alama1 and Jaouad El Harti22Laboratory of Medicinal Chemistry, Clinical and Hospital Pharmacy, Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Morocco
Abstract
Acrylic cements are used to seal orthopedic implants and, since the Eighties, these products did not cease evolving especially during not very invasive methods used to increase the stabilization of the vertebral body. The following article takes stock of the products available on the market. Thus, there exist two great groups of cements, those with high viscosity impregnated or not by an antibiotic used manually in the osseous cavities (finger packing) and, those with low viscosity developed recently and which are injected using a syringe. All these cements in common have a homogeneous chemical composition made mainly by polymers and the monomers of methacrylate of methyl (MY) added with agents of polymerization and dye specific. This composition directly influences the behavior of cement and, can modify its own characteristics especially its viscosity, the time of catch and its fatigue strength, in spite of the various methods of preparation and, of the techniques of cementing. Lastly, the selection criteria of these cements are dependent on their indications, of the type of implant has to pose and of the practices of the expert
Keywords
Orthopedic, Implants, Antibiotherapy, Homogeneous
Introduction
Orthopedic cements constitute a sure, effective and inexpensive means to ensure the fixing of the articular implants. In orthopedy, the term “cement” indicates a formed chemical body by two principal polymeric components: The methylmethacrylate (MMA) and the polymethyl methacrylate (LDC) whose polymerization allows the fixing of an implant.
Acrylic cements can be classified according to their viscosity (high or low), of their composition (with or without antibiotic) and their indications. One thus distinguishes cements of sealing of the orthopedic implants (cement of fixing) and cements used in the treatment from vertebral compressing (technical by vertebroplasty percutaneous or cyphoplasty by small baloons). Cements phosphocalcic used as osseous substitutes (cements of filling) are not approached in this article [1].
Various types of cements
Classification according to viscosity
Osseous cements are generally divided into two categories: Cements with high viscosity, and those with low viscosity. These two types of viscosity are related to two latest things of use: Cements with high viscosity [1], oldest, are introduced manually into the osseous cavities (finger packing) whereas cements with low viscosity, developed later, have the advantage of being able to be injected with a syringe.
Classification according to the composition
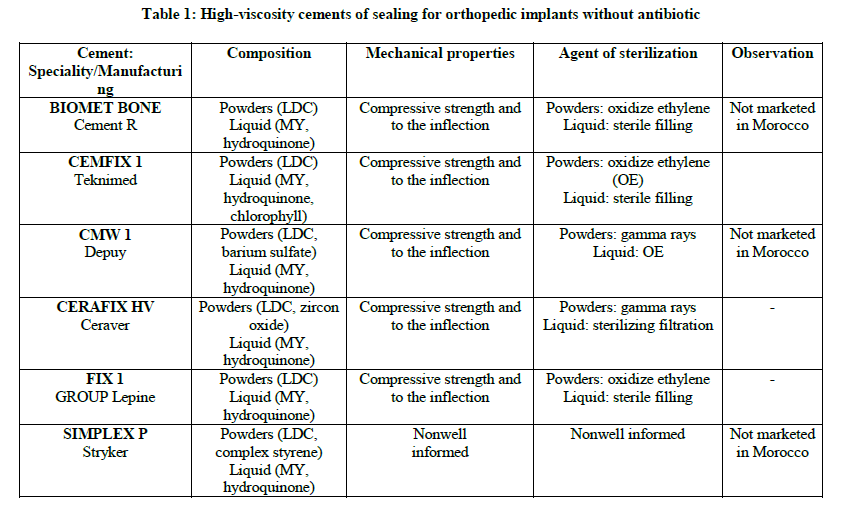
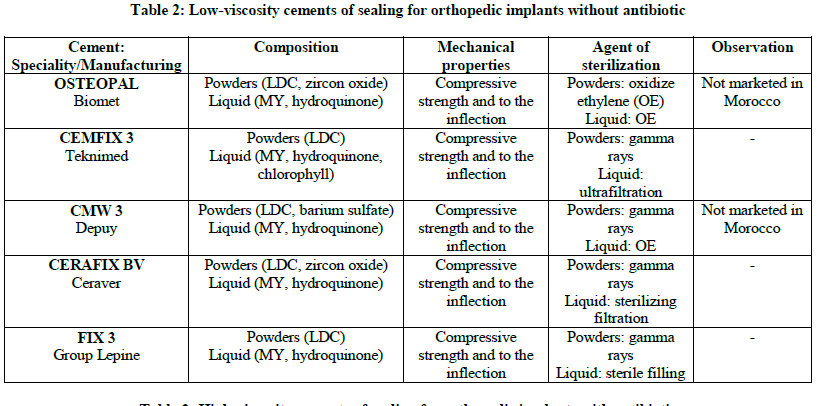
One distinguishes cements with and without antibiotic, they are registered in France on the list of the products and refundable services (LPPR) according to the absence or the presence of antibiotic (Tables 1-4) [2].
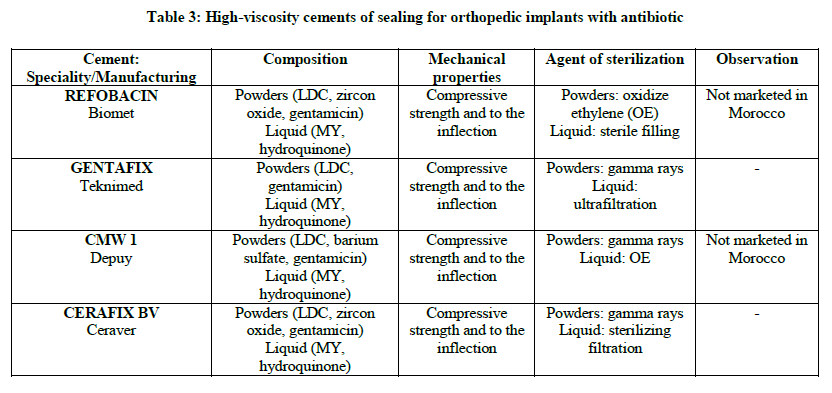
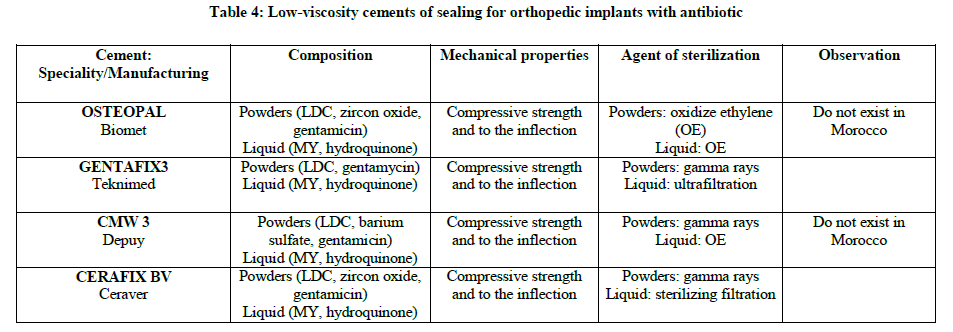
Osseous cement can be used like stamps local antibiotherapy in immediate per and post-operative period. It allows the antibiotic concentration the immediate periphery of the implant, in particular the level of bone and cartilaginous tissues difficult to reach per general way and particularly sensitive to the bacterial contamination. It was thus shown that an antibiotic administration per systemic way combined with the use of cements charged with antibiotics leads to a reduced probability of revision.
All the antibiotics in osseous cement are not adapted to a local therapy. Various criteria of clinical effectiveness are described: The spectrum of activity, the bactericidal effect even with weak concentration, the pharmacokinetic one of salting out of antibiotic, the reduced development of resistance, low allergenic potential, the incidence reduced on the mechanical characteristics of cement, chemical and thermal stability, and solubility in water.
The aminosides, and more particularly the gentamicin [3], became the antibiotics of reference for osseous cements since the beginning of the Seventies. Gentamicin, even after several years of use, continuous with being effective, with a sensitivity of the germs which remains higher than 90%.
One also finds cements containing tobramycin or erythromycin.
Present in small quantity (0.5-1 g) and mixed in a homogeneous way, the antibiotic has only little incidence on the biomechanical properties of cement. The pharmacokinetic one of salting out of antibiotic is proportional to the absorbent potential of cement, its surface and depends on the homogeneity of distribution of antibiotic in cement. The pharmacokinetic studies show the systemic absence of passage of the aminoside [3], thus limiting the side effects nephrotoxic and ototoxic. In the first years, the antibiotics were mixed extemporaneously with cement with the surgical unit to make it possible to the surgeon to adapt antibiotic according to the situation met. However, this technique exposes at the considerable risks: modification of the reaction of polymerization (delay or acceleration of the reaction), lengthening of the handling time of cement, degradation of antibiotic with loss partial of activity, reduction in mechanical qualities of cement, with increasing risk of unsealing of the prosthesis and nonhomogeneous distribution of antibiotic in the polymerized matrix. This is why pre-additives antibiotic cements by manufacturing are preferred today.
Classification according to their indication
One distinguishes on the clinical level several types of cements:
Cements of sealing of the orthopedic implants
Acrylic orthopedic cements are used in particular surgery of replacement. They allow the fixing of orthopedic implants to cement with the bones at the time of arthroplasties partial or total of hip, or knee for example. They have for primary function to link durably and in safety prosthesis with bone tissue. They constitute a biocompatible material which distributes the load supported by the prosthesis on a large surface of bone tissue. There exist two types of sealing, in particular in the case of the prostheses of hip: It is a sealing additional, one uses prosthesis “Self-locking” which one supplements with a fine layer of cement, or one uses a small prosthesis that one surrounds by a significant amount of cement, one then entrusts the constraints to the cement coat.
Cements with antibiotics allow the fixing of orthopedic implants in the bone at the time of interventions among patients at the risk infectious (general state deteriorated, malnourished, diabetic, lung infections or urinary, osseous brittleness) or at the time of re-interventions for sepsis developed on prostheses.
Cements used in the treatment of vertebral compressing
Since the years four twenties, orthopedic cements are also used during not very invasive methods of increase - stabilization of the vertebral body. One speaks about vertebroplasty and more recently about cyphoplasty.
The percutaneous vertebroplasty [4], still called “percutaneous vertebral increase” was born in 1981.
It consists in injecting, under radiological control, of cement of the LDC with strong pressure by a percutaneous needle through the pedicle directly in the spongy bone of a fractured vertebral body. The objective of this technique is to relieve the pain and to increase mobility and secondarily to stabilize the vertebral body. This technique does not aim to reduce the fracture, or to decrease the associated rachidian deformation. It presents various disadvantages and in particular rather frequent cement escapes in the adjacent zones to the vertebral and remote cops by embole.
These escapes depend on the technique of injection of cement but without any clinical consequence. In addition, the vertebroplasty increases the risk of fractures of the close vertebrae. The indications of the percutaneous vertebroplasty are vertebral compressing osteoporotic, the symptomatic tumors and symptomatic vertebral metastases and vertebral angiomas.
The cyphoplasty (or kyphoplasty), born in 2001, is a mini surgery invasive derived from the vertebroplasty. It aims to restore the height of the vertebral body, and thus to reduce the angle cyphotic, while controlling best the risk of escape of cement. This technique is characterized by the realization of a cavity aiming at correcting the vertebral deformation before the injection of cement. This cavity is created either using small baloons (two per vertebra) which one inflates after insertion in the vertebra with a product of radio operator contrast opaque, or using the device sky Bonne Expander System (manufactured by the company Disco Tech), introduced in closed configuration, then condensed under fluoroscopy until the form wished by rotation of the handle. The purpose of these two devices is to push back the spongy bone on the edges of the vertebra and to thus create a cavity by restoring the vertebral anatomy. They are then withdrawn from the cavity and filled by viscous orthopedic cement with low pressure, thus fixing the fracture.
The cyphoplasty allows a significant reduction of the consumption of analgesics and a return to a normal activity. She has various advantages compared to the vertebroplasty; in particular she decreases the risks of escapes of cement out of vertebral body and their possible complications, and corrects dorsal kyphosis partially. She is indicated in the reduction of the vertebral fractures by thoracic and lumbar compression painful and whose deformation requires a correction. These fractures can be of origin osteoporotic, cancerous (multiple myeloma) osteolytic metastatic tumors) or traumatic.
The cost of this intervention remains higher than that of the vertebroplasty. It differs however according to the technique used [5,6].
Chemical composition
Although the relative composition of the reagents varies according to the marketed specialties, it comprises a common base. Osseous cements are composed by the mixture of a powder and a liquid made up respectively of polymers and monomers of Methyl methacrylate (MMA).
The powder is mainly made up of polymerized grains of LDC. It also contains an activator of the reaction of polymerization: The benzoyl peroxide (PBO) and, generally, a radiological darkening agent: The zirconium dioxide (ZrO2) or barium sulfate (BaSO4) which makes it possible to visualize the interfaces bone - cement and cement prosthesis with the X-rays. The chlorophyll, used like dye, can possibly be added in order to facilitate visualization in particular during the elimination of cement in the event of recovery. An antibiotic can also be added in an optional way by the manufacturer.
The principal ingredient of the liquid and the monomer of MMA. Cement cannot be carried out starting from the only monomers of MMA because polymerization would be too much long and incompatible with the “timing” of an intervention. Moreover, the heat emission and the retraction of polymer (up to 21%) would be too important supporting the unsealing of the implants. For these various reasons, the adoption of composite phases (MMA+copolymère) was retained. The liquid phase also contains an activator necessary to polymerization, the NN dimethylparatoluidine (NR, NR DMPT). It can also contain a liaison officer: the methacrylate of butyl (MABU). The liquid can be stabilized by a modest amount of hydroquinone, which prevents that the reaction of polymerization does not start for the period of storage. Chlorophyll can also be added to the liquid phase.
Reaction of polymerization
The reaction of polymerization can break up into four stages:
Phase of mixture
The phase of mixture must make it possible to obtain a homogeneous paste starting from the two components, powders and liquid, it differs according to the type of selected cement. For some, it is necessary to add the liquid to the powder, whereas for others, the note indicates an opposite procedure. The instructions provided by the manufacturer must thus be strictly respected if one wishes to optimize qualities of material. The differences in composition of each cement explain the differences in behavior at the time of the phase of mixture. Certain cements are immediately smooth and liquid whereas for others it is necessary to wait a certain time. To avoid any problem during handling, the surgeon must be familiarized with the behavior of cement used.
Phase of waiting or rest
After setting in contact of the two components, it occurs a dissolution partial of the powder in the liquid and a swelling of its particles. At this moment, cement sticks to the gloves and cannot be handled by the operator if the preparation and the injection are made manually. A method of determination of the sticking phase is fixed by the standard ISO 5833, this phase is regarded as finished when cement does not adhere any more to one glove latex not powdered.
The viscosity of cement must be taken into account, most cements available claim a rest period before reaching the level of viscosity necessary for the installation. The rest period must thus be respected with the systems of modern presentation and injection. According to the ISO standard, the latency after mixture must be five maximum minutes for cement of standard viscosity.
Phase of injection or work
During this phase, cement is in a pasty intermediate state which allows handling it during a few minutes: it does not stick any more to the gloves, it is malleable and homogeneous. It is then introduced into the osseous barrel either using a syringe or with the hand by small successive amounts. The implant is set up in the osseous cavity, maintained motionless and the cement excess is eliminated. During this phase, the viscosity of cement must be sufficiently high to resist the blood pressure of the patient, but also sufficiently low so that cement interpenetrates the spongy cells essential condition with the stability of cement in the bone [7].
Phase of hardening
During the phase of hardening the final polymerization of the monomer occurs. The viscosity of cement becomes too high to allow the introduction of the implant. However continuous cement to have a certain viscous behavior and can still become deformed under the load. It is thus recommended to expect the end of the process until final hardening of cement and to check the state of hardening on the patient.
The time of catch is the time passed between the mixture (state liquid) and the moment when cement starts to harden. The length of the stages depends on the room temperature and the chemical composition of cement. During polymerization, it occurs a release of heat proportional to the volume of cement and a mechanical withdrawal [7].
Methods of preparation of cement
There exist various methods of preparation of cements [7]. These methods were developed to improve the fatigue strength of cements, at the origin of aseptic unsealing. In what concerns us, one will be satisfied to develop the manual technique.
The manual preparation in a bowl consists in mixing the powder and the liquid in a plastic container during 1-2 min with a spatula at 1 to 2 turns a second. It constituted, at the beginning of the use of osseous cements standard procedure of mixture. It is not any more the case today since the applications of the novel methods which make it possible to better control the variations of homogeneity and porosity related to the person carrying out the mixture. She remains however used because of her very weak cost.
Properties and characteristic of cements
Sterility
The sterility of cement is essential for its use in surgery [8].
Radio opacity
Radio opacity makes it possible to control the use of cement. She is strongly wished in particular, in vertebroplasty. The visualization of cement is indeed essential there for a use in full safety, particularly in the event of tumor.
Viscosity
It is the resistance of a fluid to the deformation. A material has a viscosity low and regarded as fluid, whereas a viscosity high translates a pastier consistency. Osseous cements are generally divided into cements high and low viscosity. There does not exist however precise definition high or low viscosity, also certain cements of high viscosity are sometimes presented as being of average, standard or intermediate viscosity. In addition the viscoelasticity of cement varies during polymerization, which makes difficult any measurement and quantified appreciation. The standard ISO 5833 establishes a rather vague measuring criterion: the penetration of cement in standardized pores.
The viscosity of osseous cements is primarily given by the chemical composition and by the ratio/liquid powders. These parameters should not however be modified into preoperative with an aim of changing viscosity since they would also modify other characteristics (mechanical resistance in particular). On the other hand, it is possible to modify the viscosity of cement while exploiting the temperature. It can thus be necessary to cool cement for the use of system of mixture, in particular for cements with high viscosity. The preliminary refrigeration implies a deceleration of the chemical reaction and a reduction of the viscosity of cement which becomes easier to handle and of better quality per reduction of its porosity. It is necessary however to keep in memory that it delays the phase of handling and hardening of cement.
The viscosity of cements comprises some practical consequences thus. The mixture and the installation of cement at base viscosity seem easier and more practical. Moreover, certain particular indications, like the vertebroplasties, need cements with low viscosity, because of their mode of introduction.
Mechanical properties
Osseous cement must distribute the load supported by the prosthesis on a large surface of bone tissue. IT acts like a shock absorber. It is thus prone to various constraints, more in the complex months, at the same time static and dynamic (inflection, traction, rotation, compression). Some methods evaluations in vitro were given in the standard ISO 5833 in order to test the mechanical resistance of osseous cements. The limiting values of these tests are the following ones: Modulate inflection (module of Young° 1800 millipascal (Mpa) minimum, flexural strength 50 minimum Mpa, compressive strength 70 minimum Mpa.
These values are respected by all marketed cements.
Additional static tests are sometimes carried out by certain manufacturers like resistance to lengthening, the shock resistance, or resistance in fatigue it (behavior of material under a dynamic head), but the methods all are not standardized and make the comparison of cements difficult.
Porosity
Acrylic osseous cement is a material more or porous month. The pores come either from the air imprisoned in cement at the time of the mixture or during the evaporation of the monomer during the exothermic reaction, or they are related to the phenomenon of shrinking of cement during polymerization.
The level of porosity thus influences the mechanical characteristics of material its stability. For a few years, all the efforts have thus been directed towards the reduction of the number and of size of the pores with in particular the application of new methods of mixture (mechanical, vacuum or by centrifugation) and controls it temperature of storage of the liquid monomer before the mixture. The role of the pores in the long-term stability of cement however is discussed.
Properties related to the reaction of polymerization
During polymerization, it occurs a release of heat proportional to the volume of cement and a mechanical withdrawal.
The exothermy varies according to the chemical composition of cement, of the ratio powders/liquid, of the radio operator darkening agent, and of the report/volume surfaces. It results from it an increase in temperature in cement during its phase in hardening which may be the cause of implant unsealing by osteonecrosis. In vitro, this maximum temperature oscillates between 60 and 80°C, according to the standard ISO 5833. In vivo, this temperature and much lower than (40-46°C), because the reduced thickness of the layer of cement, peripheral vascularization, and heat exchange with the vital prosthesis itself and fabrics. A room temperature of 20 with 23°C and the use of the more effective modest amount of cement distributed well between the bone and the part to be sealed are recommended to limit the extent of the exothermicity [9].
Factors influencing the characteristics of cements
Composition
The composition of cements is variable according to the manufacturers. It varies according to the relative proportions of the various components, the quantity of monomers, the additives, the rate of catalyst and initiator, the polymerized type of pre chain and the molecular weight of copolymers.
The composition conditions the behavior of cement thus and influences its viscosity, and the time of catch.
The additives can modify mechanical qualities of the mixture. Although wished, the products of contrast decrease the compressive strength. The poly (methyl methacrylate-styrene) (PMMA/ST)) increase the handling time of the pasty mixture. The methacrylate of butyl (MABU) decreases thermal rise and modifies the modulus of elasticity.
Technical of sterilization and molecular weight
The molecular weight (MW) influences the mechanical characteristics of cement. It depends on the polymer powder and polymerization on MMA. It is influenced by the process of sterilization used: sterilization by reduced gamma rays to a significant degree the MW of polymer whereas sterilization under ethylene oxide does not have any influence on this one. Cements with low MW present some disadvantages and in particular a month good fatigue strength [9,10].
Techniques of cementing
The experiment of the use of osseous cements made it possible to object of the essential factors the long-term improvement of the stability of the implants. One speaks about “modern technology of Cementing”. This one is often more determining for the result than is to it the choice of the implant. Thus, independently of the method of mixture, several conditions are necessary for an optimal and reproducible cementing.
The setting under pressure of cement makes it possible to increase its penetration in bone tissue and the shear strength with the interface.
The washing of the barrel diaphysaire avoids the mixture of the blood of the medullary cavity with cement and thus of the modifications of its mechanical properties. It also makes it possible to improve the interpenetration of cement in the bone thus to decrease the rate of unsealing and to reduce the risks of lubricating embolism. The retrograde injection of cement using a long nozzle clearly showed its advantages.
Lastly, the centering of the prosthesis in the medullary canal, in the case of prosthesis of hip, makes it possible to preserve the integrity of the coat of cement and to maintain a thickness minimum of cement.
Material of mixture and installation
Cement bowls
The cement bowls are plastic polypropylene containers, generally, used for the manual preparation of cement by mixture of the components (powder and liquids) using a spatula.
Systems of vacuum mixture
There exist various types of devices of vacuum mixture which are characterized by the depression applied (5-100 kPa), the method of mixture (by longitudinal movements and/or rotation), the capacity of the device, the type of agitator (pallet, spatula…) and the time necessary (60-150 s).
Syringes with cement or injecting guns
The injecting gun allows the setting under pressure of cement and thus improves the penetration of cement in bone tissue.
Diaphyseal obturators
The diaphyseal obturators make it possible to seal the medullary cavity before the introduction of acrylic cement. They limit the progression of cement in the diaphyse, condition its setting under pressure and ensure the protection of fabric will intra medullary thus avoiding the medullary remains passage in circulation. A compromise must however be found between a too tight obturation likely to manage an overpressure supporting the remains passage of bone marrow in blood circulation and a too permeable stopper leading to the appearance of cement escapes.
There exist many types of diaphyseal obturators of size and different forms, primarily made up of polyethylene, gelatin, or copolymers of synthesis. One thus distinguishes the resorbable plugs, and the non-resorbable plugs. The resorbable plugs are completely reabsorbed after a few days in three months and have many advantages. They facilitate the operations of recovery and make it possible to minimize the loss of bone during the shrinking of cement. In addition, they do not present the remains of wear generally met with the non-degradable synthetic obturators. Lastly, the gelatin obturators have specific properties of elasticity allowing an optimal obturation of the medullary cavity as well as a better resistance to the setting under pressure of cement. Contrary, one synthetic plastic obturators more rigid tends to let pass cement.
Selection criteria of cements
The cemented articular implants, in particular of hip, are less and less frequent, the cemented arthroplasty remains however very effective.
For that, there exists a great choice of cements with or without antibiotic, high or low viscosity having various characteristics. Choice is function of case to treat (infected or not), of type of implant to pose (same cement will not be used according to whether one poses prosthesis of knee or hip), technique of mixture and installation, methods of use of cement (time of catch…), and of the practices of the surgeon. It is thus necessary to be able to have a range of cements to adapt according to the case to treat. Liquid cement for a good diffusion, between the osseous spans will be preferred for a stem of prosthesis of hip; pastier cement which does not run will be used for cotyle. In the same way in vertebroplasty and cyphoplasty, cement will have to be sufficiently fluid to penetrate in the trocard and between the fractured osseous spans.
The clinical results resulting from the Swedish National Registers and Norwegian from Arthroplasty from hip show better rates of survival for the implants fixed with cements at high viscosity compared to those fixed with cements at low viscosity. The difference in results between these cements is not yet well understood. One of the reasons could be the non-respect of the instructions of handling, particularly the respect of the timing of the phase of work. Whereas cements with low viscosity claim to be used in a precise timing, cements with high viscosity are much more “tolerant” and authorize more reproducible results [11].
Conclusion
Orthopedic cements represent a very effective means easily allowing the fixing of the plantable medical devices in traumatologic and orthopedic surgery. Nevertheless, the difference as a result between cements is done after several years and it is important to take account of the practices of surgeon in the choice of the products. This one is attached on the one hand to mechanical qualities of cement, its mechanical resistance, and on the other hand with the aspects of use of cement, in particular to easy preparation and handling.
References
[1] P. Bourget, P. Cottin, A. Lesne, Hospital Monitor., 1990, 30, 8-15.
[2] K.D. Kuhn, R. Specht, Orthopedic., 2003, 126, 6-13.
[3] P. Davelu, Pharmacy., Lyon, 2000.
[4] A. Fisher, Canadian Coordinating Office for Health Technology Assessment, 2002, 31.
[5] A. Cotten, A. Gangi, J.D. Laredo, G. Mastretti, J.Y. Nordi, N. Passuti, Le Quotidien du Médecin., 2005, 7837(2):8.
[6] J.L Leflot, La cyphoplastie [online]. Available on: <http://www.ortholef.com/cyphoplastie/> (Accessed 01.12.2016)
[7] D. Chauveaux, Orthopedic., 2003, 126, 1-5.
[8] S. Breusch, Orthopedic., 2003, 126, 18-26.
[9] G.H.I.M. Walenkamp, D.W. Murray, Springer-Verlag Berlin Heidelberg, 2001.
[10] J. Caton, J.L. Prudhon, J.C. Aslanian, B. Ritz, Review of Orthopedic Surgery., 2002, 88, 767-76.
[11] E. Carré E, C. Delphine, The Hospital Monitor., 2006, 184, 25-38.



